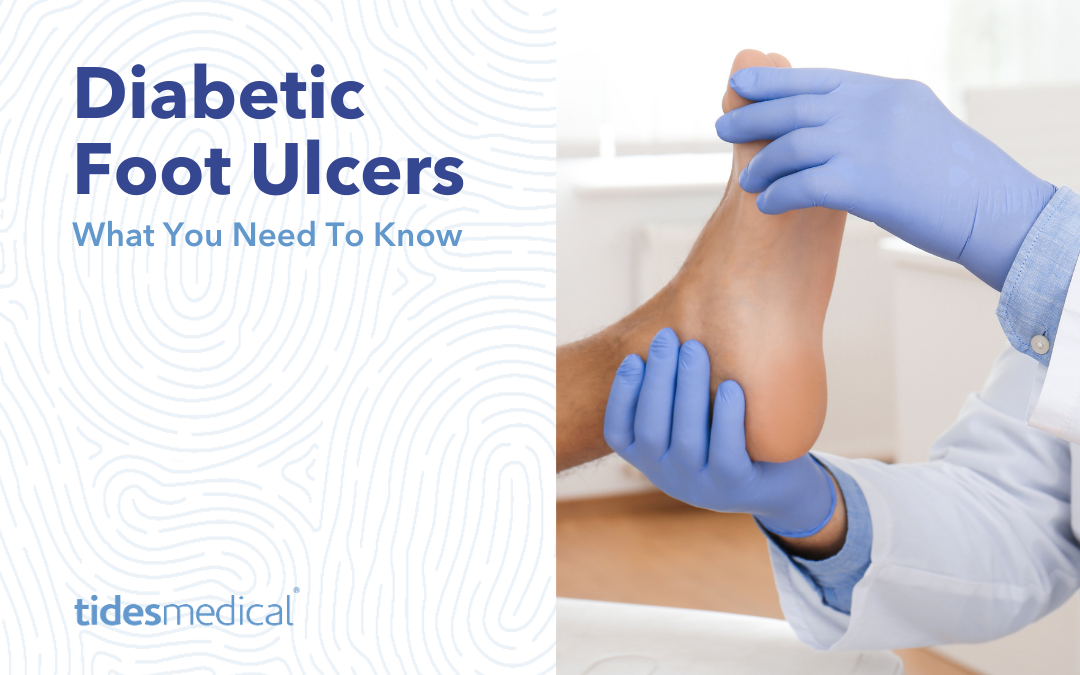
Did you know that every 1.2 seconds (1), someone develops a Diabetic Foot Ulcer? How about that every 20 seconds (1) an amputation occurs due to a diabetic foot ulcer and that one in every 4 diabetic foot ulcers result in an amputation? (3) Although anyone with diabetes can develop these foot ulcers, they are a more common complication when diabetes is not managed through things such as diet, exercise, and insulin. The purpose of this article is to dive into exactly what diabetic foot ulcers are, how they develop, tips on preventing these diabetic foot ulcers and possible treatment options.
What is a Diabetic Foot Ulcer?
The American Diabetic Podiatric Medical Association defines a diabetic foot ulcer (DFU) as an open sore or wound that is commonly found on the bottom of the foot of individuals with diabetes. They are formed when skin tissues break down exposing skin tissue layers underneath. These ulcers are most common under the big toe and on the balls of your feet and can impact your feet deep down in the foot, all the way to the bone.
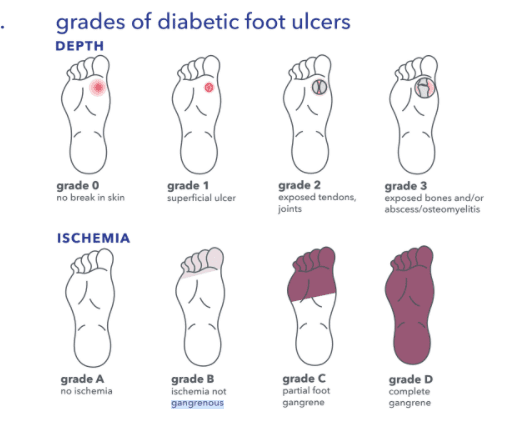
Foot Ulcer Classifications
Treatment plan and follow up will be dependent upon proper classification after evaluation. Grade is broken down by depth and ischemia. View the image below for a visual on each grade of diabetic foot ulcers. The depth of the wound is first evaluated; grade 0 is when there is no break in the skin, grade 1 is for a superficial ulcer, grade 2 is when tendons or joints below the skin tissue layers is exposed, and a grade 3 is when the ulcer has affected the foot all the way down to the bone. Grade three is the most severe of the grades and bone and or abscess/osteomyelitis is exposed. After the depth has been determined, your physician will grade by the presence (or absence) of infection and ischemia. Ischemia is the inadequate blood supply to that part of the body. Grade A would indicate no ischemia, grade B would indicate ischemia present no death of body tissue, Grade C indicates partial foot gangrene (death to body tissue) and a Grade D is for complete gangrene.
Foot Care Tips To Preventing Ulcers
As mentioned above, any diabetic can potentially develop diabetic foot ulcers. BUT, proper foot care is an excellent preventative measure. Below are some tips for caring for your feet.
- Inspect your feet daily
- Wash your feet in lukewarm (not hot) water.
- Be gentle when bathing your feet
- Moisturize your feet but not between your toes.
- Cut your nails carefully
- NEVER treat corns or calluses yourself
- Shake out your shoes and feel the inside before wearing
- NEVER walk barefoot
- Get periodic foot exams.
- Talk to your physician about proper footwear.
Signs of Diabetic Foot Ulcers
Get to know your feet! Inspect your feet regularly to look for any potential causes for concern. If you notice any changes or see anything of concern, contact your doctor, nurse, or podiatrist, especially if you have developed any new sores, wounds, or swelling. Some changes to keep an eye out for include but are not limited to: changes in blood supply and changes to nerves. If you see changes in discoloration, experience pain/cramps, or notice wounds/sores, these could be a sign of blood supply issues and should be brought to your doctors attention. If you notice tingling, numbness or hard skin, these could be signs of nerve issues that should be brought to your doctors attention.
Treatment Options
Treatment will depend both on the severity of your foot ulcer and the cause. It is important to get with your doctor about your personal situation for the best treatment options. Tides Medical offers a line of amniotic tissue products. These incredibly versatile wound coverings do not require sutures, are strong enough for implantation yet gentle enough to keep natural biologic factors. These are an excellent wound covering option for patients with diabetic foot ulcers, pressure ulcers, venous stasis ulcers and more. Ask your doctor if you would be a good candidate for Tides Medical wound covering products.
1.Armstrong DG, Kanda VA, Lavery LA, Marston W, Mills JL, Boulton AJ. Mind the gap: Disparity between research funding and costs of care for diabetic foot ulcers. Diabetes Care. 2013;36(7):1815-1817. 2. SmartTRAK 3. Pemayun, T.G.D., Naibaho, R.M., Novitasari, D., Amin, N., Minuljo, T.T., Risk factors for lower extremity amputation in patients with diabetic foot ulcers: a hospital-based case–control study. Diabetic Foot & Ankle, 2015. 6:10.3402/dfa.v6.29629. doi:10.3402/dfa.v6.29629. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4673055/ (accessed 8/5/2016)


 Marc Stemler,
Marc Stemler,  Mora Melican, Ph.D., VP of Operations, Research & Development
Mora Melican, Ph.D., VP of Operations, Research & Development LESA CATALON,
LESA CATALON, DAVID CASTILLE,
DAVID CASTILLE,

 JOSH WILLETT,
JOSH WILLETT, JEFF MONTGOMERY,
JEFF MONTGOMERY, MIKE RIDDLE,
MIKE RIDDLE, BENJAMIN KIMBALL,
BENJAMIN KIMBALL, DOUG PAYNE,
DOUG PAYNE, JOE SPELL,
CEO
JOE SPELL,
CEO